Hypnosis and pain research (hypnotic analgesia research)
Reduction or removal of pain (analgesia) is one of the most dramatic effects of hypnosis and suggestion. This page contains information about research conducted to find out how hypnotic analgesia works. For more information about how effective hypnosis is for treating pain see the clinical pain section.
Hypnotic analgesia research
Hypnotic analgesia is dependent upon suggestion
A key fact is that the induction of hypnosis by itself does not generate significant pain relief. It is the suggestion inside a hypnotic framework, or at least the expectation of pain relief which leads to reduction of pain. A number of studies have specifically assessed pain relief following a hypnotic induction, or the induction of hypnosis + specific suggestions (Knox et al, 1974; Zachariae et al, 1998). The induction of hypnosis alone is not generally sufficient to achieve significant pain relief.
Hypnotic analgesia is not dependent upon endorphins
One early explanation for hypnotic analgesia was that it could be dependent upon the body's natural painkilling system - the endogenous opiate system. This was tested experimentally by Goldstein & Hilgard in 1975. They administered the drug Naloxone, which blocks the effects of opiates, to participants experiencing hypnotic analgesia. They found that hypnotic analgesia was not significantly affected by this inhibition of the opiate system, indicating that another mechanism must be responsible. Weitzenhoffer also pointed out that endogenous opiates are an unlikely source of hypnotic analgesia because of the latter's quick reversibility, and specificity (i.e. hypnotic analgesia can be directed at one location, leaving another unaffected).
Hypnotic analgesia is not dependent upon relaxation
Since many hypnotic inductions contain elements of relaxation it has been proposed that any pain relieving properties of hypnotic suggestion could be due primarily to a relaxation response. However, this hypothesis has been tested experimentally. Miller and colleagues (1991) gave analgesia suggestions to two groups of participants: the first group were hypnotised using a traditional relxation induction, the second group were hypnotised using an active-alert induction whist riding a stationary exercise bicycle. They found that the amount of pain relief experienced by each group was equivalent, contradicting the idea that hypnotic analgesia is simply the result of relaxation.
Hypnotic analgesia does not seem to be dependent upon imagery
Despite imagery often forming a key component when hypnosis is used clinically, one study has directly tested the additive benefits of imagery to hypnotic analgesia suggestions. Hargadon and colleagues (1995) tested 66 high hypnotizables in 3 conditions: baseline, hypnotic analgesia with imagery encouraged, and hypnotic analgesia with imagery proscribed. Pain was rated as significantly less in the two hypnotic analgesia conditions compared to baseline, and there were no significant differences between the two treatment conditions. In contrast to this evidence, many clinicians report that the use of imagery in hypnosis is particularly useful in helping clients to engage with treatment, more work is needed to clarify the precise role of imagery in hypnotic responding.
What hypnosis can tell us about pain itself
As well as telling us more about hypnosis and suggestion a number of studies have had a feed-back effect and told us more about the nature of the pain system in humans.
Modulation of pain unpleasantness independent of sensory components
In 1997 Rainville and colleagues published a landmark study which investigated the neural correlates of pain in humans. Using positron emission tomography (PET) they measured brain activity in a group of highly hypnotisable subjects while they had their hand immersed in either neutral (35ºc) or painfully hot (47ºc) water. Hypnotic suggestions were given for participants to experience increased and decreased pain unpleasantness and verbal pain reports were taken.
The figure below shows the area of the anterior cingulate cortex found by Rainville to have activity which correlated with the reported unpleasantness of the pain. Interestingly, as early as 1962 this area of the brain had been thought to be involved in the perception of pain unpleasantness.
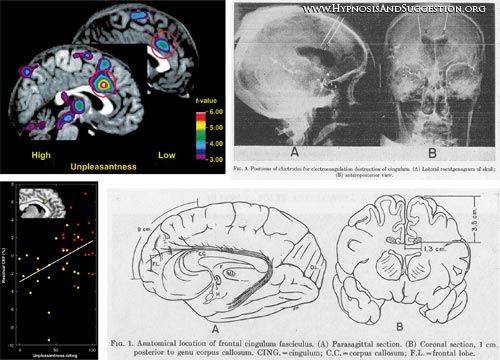
Figure: Colour images show the area of anterior cingulate cortex (ACC) whose activity correlated with perceived unpleasantness in Rainville et al (1997). Black and White images from Folz & White (1962) showing probe positioning to produce lesions in the same region of the ACC which produced reductions in perception of pain unpleasantness.
Using hypnosis to generate pain in the absence of a noxious stimulus
In a study investigating functional pain (pain without an obvious physical cause) Derbyshire and colleagues (2004) published a study investigating brain activity in highly hypnotisable participants while they experienced physically-induced (PI), hypnotically-induced (HI), or imagined pain. Participants were pre-selected for their ability to hallucinate a sensation of pain. In both the PI and HI pain conditions participants were led to expect that an electrical heat probe attached to their hand would heat up to become painfully hot. However, painful heat was only delievered in the PI condition. In the HI condition the probe was not switched on, but participants reported feeling varying strengths of pain.
In both the PI and HI conditions signficant activations were reported in key areas of the pain network, including the thalamus, insula, anterior cingulate cortex, and prefrontal cortex. Additionally, activation was observed in the HI condition in the primary somatosensory cortex. Imagination of pain only resulted in minimal acitvation of the pain network. These results indicate that it is possible to experience pain in the absence of direct stimulation, and provide some evidence for direct cortical involvement in some clinical functional pain disorders. Similar results were reported in 2005 by Raij and colleagues.
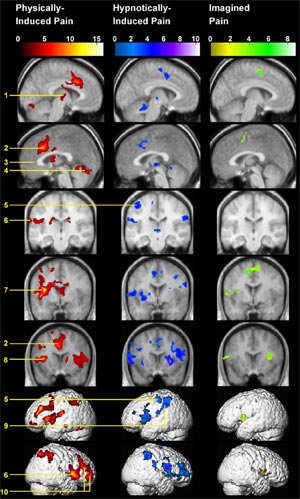
Figure: Pain activations reported by Derbyshire et al (2004) in response to physically-induced (red), hypnotically-induced (blue), and imagined (green) pain.
What is hypnosis?
Definitions of hypnosis
Types of suggestion
FAQ
Scientific theories of hypnosis
History of hypnosis
Animal hypnosis
Key people in hypnosis
Demand characteristics
Scientific research
States of consciousness
Neuroscience
Modification of suggestibility
Attention and hypnosis
Pain research
Hypnosis as a research tool
Genes and hypnotizability
What is hypnotherapy?
Is it effective?
Finding a therapist
Depression
Irritable bowel syndrome
Pain
PTSD
Smoking
Surgery
Weight loss
Hypnosis research papers
Suggestibility scales
Scripts
Videos
Forum
Organisations
Journals
Book reviews
© 2007-2019 Dr Matthew Whalley
